
Black Women:

- Each year, around 71,500 women are diagnosed with gynecologic cancers, and 26,500 die from them
- Black women are 30% more likely to develop cervical cancer and 60% more likely to die from it than non-Hispanic White women.

- Black women are also more likely to be diagnosed at a later stage and have lower five-year survival rates.

- In rural areas, Black women face a cervical cancer incidence rate almost 50% higher than white women.

- Black women are more likely to be diagnosed with uterine cancer and more than twice as likely to die from it than other racial and ethnic groups.

- Black women are also more likely to develop triple negative breast cancer (TNBC) than other ethnicities. TNBC is often aggressive and is more likely to recur within the first five years after diagnosis than estrogen receptor-positive breast cancers.

- Black women with epithelial ovarian cancer are diagnosed most often with high-grade serous tumors, the most aggressive kind.
Why Do Black Women Die Sooner From Ovarian Cancer?
- Even though they’re diagnosed less often than other groups, Black women have the second-highest chance of dying from ovarian cancer. They also live the shortest amount of time after their diagnosis. These lower survival rates hold true no matter what stage of cancer they have.
- Experts aren’t sure why Black women don’t live as long after their diagnosis. There’s ongoing research in this area. Here are some theories scientists are looking into:
- Disparities in treatment. Black people are generally less likely to have access to money, education, affordable health insurance, and quality health care. Experts largely blame this on decades of racial discrimination.
- Structural racism and other barriers to health care can affect cancer care. They can make it so Black women with ovarian cancer are less likely to get:
- Social support
- Timely treatment
- Care at a high-volume cancer center
- Optimal surgery and chemotherapy
- Treatment that follows national cancer guidelines
- Black women are also more likely to:
- Get diagnosed with advanced ovarian cancer
- Receive lower doses of chemotherapy
- Stop cancer treatment early
Medical mistrust. While Black people tend to have unequal access to care, they’re also less trusting of health professionals and medical treatment. There are well-documented reasons for this.
Other health problems. Black women are diagnosed with certain medical conditions more often than other groups. Public health experts think genes, lifestyle, and the ongoing stress of systemic racism likely all play a part. Some health issues may boost your odds of ovarian cancer or affect your response to treatment. These include:
- Obesity
- High blood pressure
- Kidney disease
- Heart disease
- Diabetes
- Higher levels of inflammation
- Low levels of vitamin D
Genetic variants. Genes are passed down through families. And there’s some evidence that Black women are more likely to inherit DNA changes involved in ovarian cancer, including the BRCA1 and BRCA2 gene mutations.Lack of representation in clinical trials. Black people are underrepresented in clinical trials. That makes it hard to know if new treatments for ovarian cancer will work as well in Black women.
What is Reproductive Cancer?
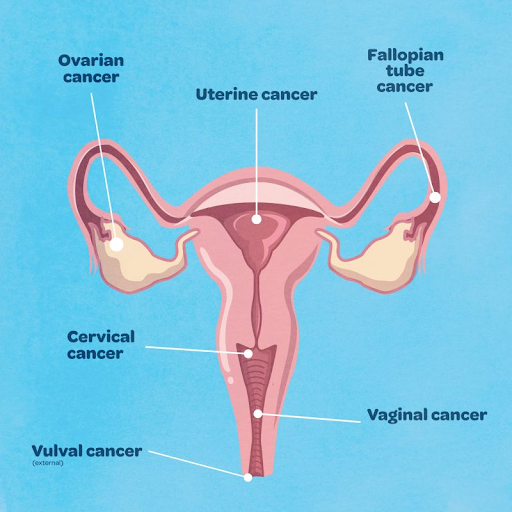
Reproductive or Gynecologic cancers are a group of malignancies that affect the female reproductive organs. They include:
- Cervical cancer: Cancer of the cervix, the lower part of the uterus
- Endometrial cancer (uterine cancer): Cancer of the lining of the uterus
- Ovarian cancer: Cancer of the ovaries, the female reproductive organs that produce eggs
- Vaginal cancer: Cancer of the vagina, the tube that connects the uterus to the outside of the body
- Vulvar cancer: Cancer of the vulva, the external female genital organs
- Gestational trophoblastic disease (GTD): A rare group of cancers that develop after pregnancy
Is breast cancer considered a reproductive cancer?
Yes, breast cancer is generally considered a reproductive cancer. Reproductive cancers are cancers that affect the organs and tissues involved in reproduction, including the: Breasts, Ovaries, Uterus, Vagina, Vulva, and Cervix.
Breast cancer is the most common reproductive cancer in women, and it is often associated with reproductive factors such as early menstruation, late menopause, and not having children. This is because these factors can increase the body’s exposure to estrogen, which is a risk factor for breast cancer.
Therefore, breast cancer is classified as a reproductive cancer due to its association with the female reproductive system and its potential impact on reproductive health.
Risk factors for gynecologic cancers vary depending on the type of cancer but may include:
- Age
- Family history of gynecologic cancer
- Human papillomavirus (HPV) infection
- Obesity
- Hormonal factors
Cervical Cancer

- Risk Factors
The primary risk factor for cervical cancer is infection with the human papillomavirus (HPV). Other factors include smoking, weakened immune systems, multiple sexual partners, early sexual activity, and having many children. In addition, a history of certain sexually transmitted infections (STIs) and exposure to the drug diethylstilbestrol (DES) during pregnancy can also increase the risk.
Here’s a more detailed look at these risk factors:
- HPV infection
- Nearly all cervical cancers are caused by persistent HPV infection.
- Certain high-risk HPV types are particularly associated with cervical cancer.
- HPV vaccination can protect against these high-risk HPV types.
- Sexual History
- Multiple sexual partners: Increases the risk of HPV exposure.
- Early sexual activity: May increase the risk of HPV infection.
- History of STIs: Certain STIs like chlamydia, gonorrhea, syphilis, and herpes can increase the likelihood of HPV infection.
Other Factors include:
- Weakened immune system: Can make it harder for the body to clear HPV infections, increasing the risk of cervical cancer.
- Smoking: Increases the risk of cervical cancer and can make HPV infections last longer.
- Exposure to DES: A synthetic estrogen medication used in the past during pregnancy, can increase the risk of a specific type of cervical cancer.
- Age: The risk of cervical cancer increases with age, but it’s also possible to develop precancerous lesions at younger ages.
- Family history: A family history of cervical cancer may also increase a person’s risk.
- Lack of screening: Not having regular Pap smears or other cervical cancer screenings increases the risk of cervical cancer.
- Having many children: Multiple pregnancies may increase the risk of cervical cancer.
2. Symptoms:
Early cervical cancer often has no symptoms. However, as the cancer progresses, common symptoms can include unusual vaginal bleeding, vaginal discharge, and pelvic pain. Other potential symptoms include painful urination, difficulty urinating, or back pain.
- Early Symptoms
- Abnormal vaginal bleeding: This can include bleeding between periods, bleeding after sexual intercourse, or bleeding after menopause.
- Vaginal discharge: This can be thick, watery, bloody, or have a foul odor.
- Pelvic pain: Pain in the lower back, pelvis, or abdomen can occur.
- Pain during sexual intercourse: Some individuals may experience pain during or after sex.
- Advanced Symptoms
- Difficulty or painful urination: Changes in urination patterns or pain while urinating can occur.
- Blood in the urine: This can be a sign of advanced cancer.
- Difficult or painful bowel movements: Changes in bowel habits, including bleeding from the rectum, may also be present.
- Swelling of the legs: This can be a sign of cancer that has spread.
- Back pain: Dull backache, especially in the lower back, can be a symptom.
- Fatigue and weight loss: Some individuals may experience fatigue or unexplained weight loss.
It’s important to remember:
- Not everyone with cervical cancer will experience symptoms.
- Regular cervical screening tests (Pap tests and HPV tests) are crucial for early detection.
- If you experience any of the above symptoms, it’s important to see a doctor for proper diagnosis and treatment
3. Diagnosis:
Diagnosis typically involves a physical exam, pelvic exam, and imaging tests such as a Pap smear, biopsy, or CT scan.
- Treatment:
- Treatment options depend on the type of cancer, stage, and overall health of the patient. They may include surgery, chemotherapy, radiation therapy, or a combination of these methods.
- Prevention:
- Regular gynecologic screenings, including Pap smears and HPV vaccinations, can help prevent or detect gynecologic cancers early on. Maintaining a healthy weight, exercising regularly, and limiting alcohol consumption may also reduce risk
Uterine Cancer
- Risk Factors:
Several factors can increase the risk of uterine cancer, including obesity, hormone imbalances (like Lynch syndrome or high estrogen levels), family history of uterine or colon cancer, and age. Additionally, certain medical conditions, like diabetes, and the use of estrogen-only hormone replacement therapy can also elevate the risk.
Here’s a more detailed breakdown:
- Estrogen exposure
- Hormone Imbalances
- Unbalanced estrogen and progesterone levels can increase the risk of endometrial cancer, which is the most common type of uterine cancer.
- Hormone Replacement Therapy (HRT)
- Long-term use of estrogen-only HRT after menopause can increase the risk of endometrial cancer.
- Early Menstruation/ Late Menopause
- Starting menstruation early (before age 12) and ending it late (after age 52) increases lifetime exposure to estrogen and raises the risk.
- Obesity:
- Fat Tissue and Estrogen:
Obesity increases the risk of uterine cancer because fat tissue can convert androgens into estrogen, leading to higher estrogen levels. - Metabolic Changes:
Obesity is also associated with changes in insulin and other growth factors, which can promote tumor growth.
- Fat Tissue and Estrogen:
- Medical Conditions and Medications:
- Diabetes: Women with diabetes have a higher risk of uterine cancer.
- Polycystic Ovary Syndrome (PCOS): PCOS, a condition characterized by hormonal imbalances, increases the risk of endometrial cancer.
- Tamoxifen: This medication, used to treat breast cancer, can increase the risk of endometrial cancer.
- Family History
- Lynch Syndrome
- This genetic condition, which increases the risk of colon, endometrial, and other cancers, is a significant risk factor.
- Having a close relative with uterine or colon cancer can also increase your risk.
- Other Factors:
- Never Having Been Pregnant:
Women who have never been pregnant may have a slightly higher risk of endometrial cancer. - Older Age:
The risk of uterine cancer increases with age, particularly after menopause. - Infertility:
Infertility or difficulty getting pregnant can also be associated with a higher risk.
- Never Having Been Pregnant:
Ovarian Cancer
- Risk Factors
Several factors can increase a woman’s risk of developing ovarian cancer. These include older age, family history of ovarian or breast cancer, certain genetic mutations (like BRCA1 or BRCA2), endometriosis, and a history of infertility or never having been pregnant.
Elaborating on the risk factors:
- Age: The risk of ovarian cancer increases with age, with most diagnoses occurring in women 50 and older.
- Family History: Having a family history of ovarian cancer, breast cancer, or colorectal cancer increases the risk.
- Genetics: Certain genetic mutations, such as BRCA1 and BRCA2, significantly increase the risk of ovarian cancer.
- Reproductive History: Factors like starting menstruation early, experiencing menopause later, never having children, or having a first child after age 30 may increase the risk.
- Medical Conditions: Endometriosis (where tissue similar to the uterine lining grows outside the uterus) and infertility can also increase the risk.
- Hormone Therapy: Taking hormone replacement therapy after menopause may also increase the risk of ovarian cancer.
- Obesity: Being overweight or obese is linked to a higher risk of ovarian cancer.
- A history of breast cancer, certain types of cancers (like uterine or colorectal), and even smoking have been associated with an increased risk in some cases.
Vaginal Cancer
- Risk Factors
Vaginal cancer is a rare type of cancer that can affect women of all ages. The following risk factors have been identified as increasing the risk of developing vaginal cancer:
- Human Papillomavirus (HPV): HPV is the primary cause of vaginal cancer. It is a sexually transmitted infection that can cause precancerous lesions on the vagina and cervix.
- Multiple Sexual Partners: Having multiple sexual partners increases the risk of
- exposure to HPV and other sexually transmitted infections.
- Smoking: Smoking damages the immune system and increases the risk of HPV infection and other cancers.
- History of Cervical Cancer or Precancerous Lesions: Women who have had cervical cancer or precancerous lesions on the cervix are at an increased risk of developing vaginal cancer.
- Diethylstilbestrol (DES): DES is a synthetic hormone that was prescribed to pregnant women in the 1940s and 1950s to prevent miscarriage. Exposure to DES in the womb can increase the risk of vaginal cancer.
- Weakened Immune System: Conditions that weaken the immune system, such as HIV and autoimmune disorders, increase the risk of HPV infection and other cancers.
2. Other Risk Factors:
- Age: The risk of vaginal cancer increases with age, History of radiation therapy to the pelvis, Certain genetic factors, and Chronic vaginal irritation.
3. Prevention:
Get vaccinated against HPV, Practice safe sex, Avoid smoking, and See your doctor regularly for pelvic exams and Pap tests.
It’s important to note that not everyone who has these risk factors will develop vaginal cancer. However, being aware of the risk factors can help you take steps to protect your health. If you have any concerns about your risk of vaginal cancer, talk to your doctor.
Vulvar Cancer
- Risk Factors
Vulvar cancer risk factors include older age (most women diagnosed are over 65), exposure to human papillomavirus (HPV) (especially certain high-risk types), smoking, a weakened immune system, and precancerous vulvar conditions like vulvar intraepithelial neoplasia (VIN) or lichen sclerosus. Other risk factors include a history of melanoma, other genital cancers, and chronic vulvar skin conditions.
Elaboration:
- Age: The risk of vulvar cancer increases with age, with most diagnoses occurring in women over 65.
- HPV: HPV, a sexually transmitted infection, is a significant risk factor, particularly exposure to high-risk types.
- Smoking: Smoking is associated with an increased risk of vulvar cancer.
- Immune System: A weakened immune system, due to conditions like HIV or certain medications, can increase the risk of HPV infection and thus vulvar cancer.
- Precancerous Conditions: Conditions like VIN and lichen sclerosus can increase the risk of developing vulvar cancer.
2. Other Risk Factors:
- Melanoma, other genital cancers (like cervical cancer), and chronic vulvar skin conditions (like lichen planus) can also increase the risk.
Gestational Trophoblastic Disease (GTD)
- Risk Factors
GTD risk factors include previous molar pregnancy, extremes of age (younger than 20 or older than 35), and a history of miscarriage. Other factors that may increase risk include a history of previous GTD, smoking, and certain ethnicities (like women from Southeast Asia).
More Detailed Explanation:
- Previous Molar Pregnancy: A woman who has had a previous molar pregnancy (hydatidiform mole) has a significantly higher risk of developing another molar pregnancy or other forms of GTD.
- Maternal Age: Being pregnant before age 20 or after age 35 increases the risk of GTD, particularly complete molar pregnancies.
- History of Miscarriage: A history of miscarriage is also linked to a slightly increased risk of GTD.
- Smoking: Smoking has been identified as a potential risk factor for molar pregnancy and GTD.
- Ethnicity: Women from Southeast Asia and those with low dietary carotene may have a higher risk of molar pregnancy and GTD.
2. Other Potential Factors:
- High levels of beta human chorionic gonadotropin (beta-hCG), large uterine tumors, and ovarian cysts can also increase the risk of GTD.
Breast Cancer
- Risk Factors
Breast cancer is a complex disease with multiple risk factors that can increase a person’s likelihood of developing it. These risk factors can be categorized as follows:
Non-Modifiable Risk Factors:
- Age: The risk of breast cancer increases with age, especially after menopause.
- Family history: Having a close relative (e.g., mother, sister, daughter) with breast cancer increases the risk.
- Genetic mutations: Mutations in certain genes, such as BRCA1 and BRCA2, significantly increase the risk of breast cancer.
- Dense breast tissue: Dense breast tissue is harder to screen for cancer.
- Race: White women have a higher risk of breast cancer than women of other races.
2. Modifiable Risk Factors:
- Hormone use: Use of hormone replacement therapy (HRT) after menopause and certain oral contraceptives can increase the risk.
- Alcohol consumption: Excessive alcohol consumption increases the risk.
- Physical inactivity: Lack of regular physical activity increases the risk.
- Obesity: Being overweight or obese increases the risk, especially after menopause.
- Early menstruation: Starting menstruation before age 12 increases the risk.
- Late menopause: Going through menopause after age 55 increases the risk.
- History of benign breast disease: Having a history of non-cancerous breast conditions, such as fibroadenomas or cysts, may slightly increase the risk.
It’s important to note that having one or even several risk factors does not mean that a person will develop breast cancer. However, understanding these risk factors can help individuals make informed decisions about their health and take appropriate preventive measures, such as regular screenings and lifestyle modifications